Work-Recovery Balance
Work-Recovery Balance ©
Most are familiar with the term ‘work-life balance’ when describing the relationship between work and personal life. For workers in or seeking recovery, adding recovery efforts to the equation creates a new wrinkle to the balancing act.
At Manifesto Health, we know first-hand that recovery and work can intersect to create a positive force of motivation and sustainability. Engaging in meaningful work can ignite that unique and deeply personal part of yourself that feels like you're contributing, being creative, and growing. Reigniting your professional sense of self can be a huge gain to the recovery side of the balance scale. At the same time, we recognize that the extremes—such as the pesky “all or nothing” thinking—are something we need to keep in check.
Striking a balance between finding purpose and meaning in your work—and leaving room for the other important spheres of your life—can be an instrumental force in sustained recovery. Engaging in fulfilling work while maintaining the persistent self-work required for recovery is what we coin, Work-Recovery Balance ©.
Work-Recovery Balance refers to the equilibrium between the sense of purpose and satisfaction derived from one’s professional pursuits, the demands and responsibilities of work, the allocation of time and energy towards personal recovery efforts, and the nurturing of all other spheres of a values-based life.
For example, working all day and night with no room for the other components of recovery (e.g., connection, health, leisure, recovery support) is not a good recipe for longevity. Likewise, attending 5 mutual aid groups per day with no room for feeling productive through meaningful work is also not a very sustainable routine (although that may be what we need in the beginning). We can’t be all work, with no recovery—the same as we can’t be all recovery, with no work. Finding the synergy in the time and effort we spend in our work—and the time and effort we spend in our recovery and other personal domains—is what Work-Recovery Balance is all about.
The truth is—work and recovery are not mutually exclusive of one another. As we discussed, there are many recovery benefits to be found in your work. Experiences like feeling creative and productive—as well as connection to your coworkers, customers, or clients—are all recovery-sustaining elements of meaningful work.
The socialization and community that’s available in the workplace is often an advantageous stepping stone for people in early recovery transitioning to contributing roles in society. Yet, balancing the lifestyle and behavior changes of substance use management amidst the demands at work is no easy task. It’s one that requires fine-tuned self-awareness and intentional practice.
If you follow Manifesto Health, then you know our stance on meaningful work as a major driver of long-term success in recovery. Of course, not everyone will find all of their life’s purpose in their employment. In fact, purpose and fulfillment will never be solely achieved in one’s occupation. There will likely be parts of our jobs, or even days or weeks of our jobs, that we don’t necessarily love or jump out of bed for. “They call it work for a reason!” as the saying goes—and a lot of the time, work feels like work. The key is choosing and creating a career path that amidst the hard work and sacrifice, can also make you feel productive, skilled, connected to others, purposeful, and contributing to something bigger than yourself.
Manifesto’s curriculum pertaining to Work-Recovery Balance offers practical guidelines on navigating the uncharted waters of balancing work-related efforts amidst recovery-related ones.
We provide guidance and support for (a) the employee navigating a successful recovery journey while continuing to contribute meaningfully at work—as well as (b) the employer in creating a Recovery-Ready workplace to effectively support its employees in or seeking recovery.
Contact us today to learn more about how Manifesto Health can help your employees become more productive, healthy, and balanced in their substance use management.
What is Peer-led Navigation?
Short answer: Peer-led navigation refers to the aspect of peer support services where individuals who have lived experience with mental health and/or substance use challenges themselves assist people in navigating the complex landscape of mental health care. These peers use their personal experiences and training to guide and support others in accessing the appropriate mental health services, resources, and information they need to address their mental health concerns. This form of support is rooted in empathy, understanding, and shared experiences, and is a valuable — yet underutilized — component of the mental health care system.
The Manifesto Health Difference: Peer navigation is not a new concept. In fact, peer navigators have been utilized as linkage to community resources and access to care in a multitude of forms such as living with complex medical conditions and reintegration post-incarceration. Manifesto’s peer specialists are especially trained to navigate people in need through the complex and fragmented process of finding clinical treatment. They have walked a similar path of seeking mental health support which gives them a deep understanding of the feelings, fears, and uncertainties that can accompany help-seeking.
Currently, access to mental health and substance use care is burdened with barriers such as an alarming supply crunch of mental health providers and months-long wait lists for clinical treatment. Manifesto’s peer specialists are equipped to keep people “warm” and engaged in the waiting period before an intake appointment. Further, our peer specialists engage people post-treatment to effectively extend the continuum of support and help sustain recovery journeys for the long run — bolstering critical processes such as integrating back into the workforce in the event of a medical leave of absence.
Importantly, when navigation services are “peer-led” in mental health care, the peer professional leads the interaction with the patient. However, peer specialists are not trained or certified to diagnose, assess, or recommend specific treatment levels or modalities. Supervision of the peer professionals by Manifesto Health’s expert clinical team enables the efficient and evidence-based triage process to treatment providers when clinical needs and criteria arise.
Peer-led navigation has demonstrated efficacy by:
- Increasing capacity to navigate service systems and advocate for coordinated and integrated care and support
- Having a peer worker provide non-clinical support to people experiencing mental health and substance use issues and supporting them while navigating the service system
- Integrating social connection within mental health care
- Addressing the broader social determinants of health and factors that contribute to distress and mental health challenges (such as homelessness or not having a primary care practitioner)
- Supporting service systems where there is a workforce shortage and/or overburdened workload of mental health clinical staff, such as underserved and rural areas
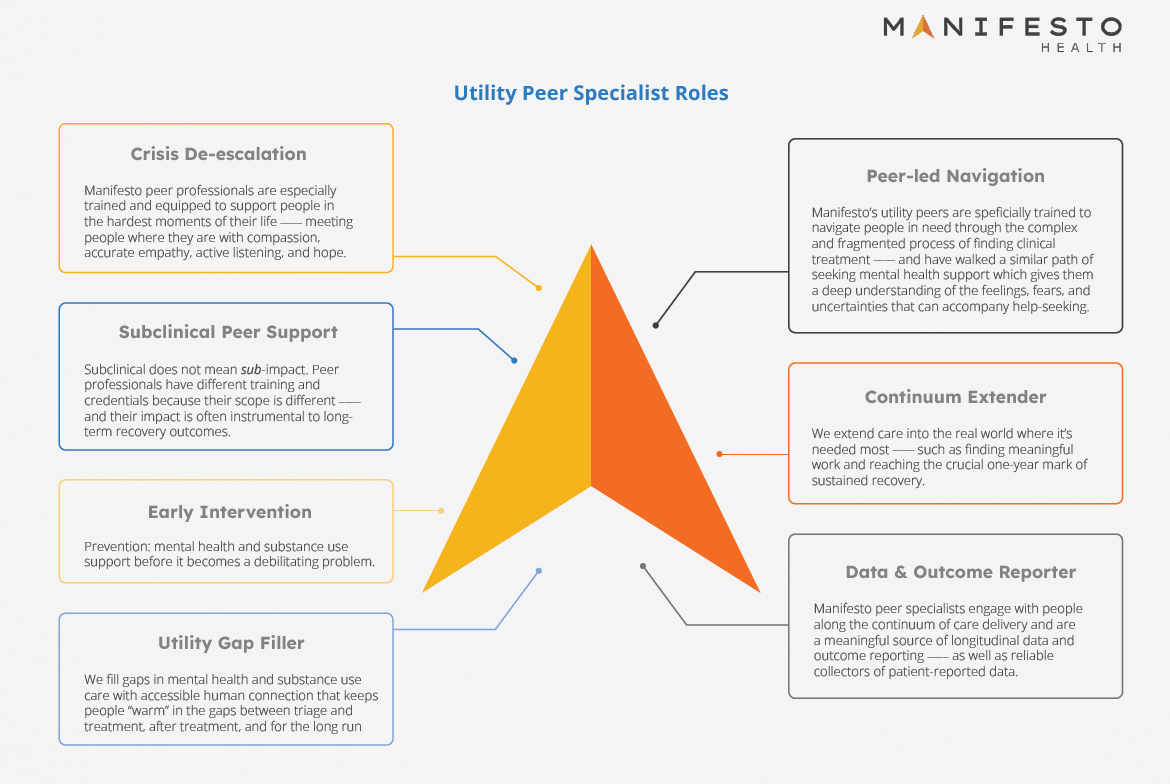
Stay tuned for more posts describing the versatile roles of Manifesto’s utility peer specialist (see graphic) such as Crisis De-escalation, Early Intervention, Data & Outcome Reporting, and more!
New Product Guide
We are excited to present our latest Product Guide for Employers!
Manifesto’s mission originated in the workplace: Building a Recovery-Ready Future for Individuals and the Companies They Work For.
Recovery-Ready is not just a stamp of approval for attending a training. It means that a company is committed to supporting its greatest asset — its people – with access to proactive mental health and substance use services within a culture of compassion — free from the barriers of stigma and disregard that have plagued workplaces for far too long.
Read on to learn how Manifesto can proactively make your organization Recovery-Ready with digital peer support and peer-led navigation services that enhance accessibility to human connection and fill costly gaps in substance use and mental health care.
Recovery Ready Summit
We were honored to participate in the Recovery Ready Summit hosted by the Independence Blue Cross Foundation and their meaningful partnership with The Association of Recovery in Higher Education (ARHE).
As a direct result of IBX Foundation's mission to establish and expand recovery support on college campuses, Pennsylvania is now leading the nation in the number of Collegiate Recovery Programs. And the work is just getting started — colleges and universities located in Southeastern Pennsylvania interested in establishing or expanding a collegiate recovery program are encouraged to apply now for grant funding.
Our CEO, Dan Hilferty, Jr., and Head of External Affairs, Patrick Flynn, presented on Manifesto's peer support services for individuals in recovery entering the workforce — as well as our recovery-ready workplace solution that help employers create a company culture that openly supports employees in or seeking recovery.
Treasure Coast Opioid Summit
We were thrilled to join the conversation at the Treasure Coast Opioid Summit in Martin County, Florida.
Our own, Dr. Mullen, presented with other subject matter experts including David Nash, PhD, PMP, Eric J. Gremminger, ICADC, SAP, James Carroll, moderated by Micah Robbins.
Patrick Mullen, Psy.D. spoke about the complexity of the opioid crisis and its intersection at many contributing issues such as underlying mental health conditions, trauma, disconnection, economic and educational disparities, stigma, discrimination, access to healthcare, limitations in mental health care funding/reimbursement, illicitly-manufactured synthetic opioids, and more.
While no single solution can solve the opioid crisis, Manifesto's peer support platform is aiding in the efforts to expand the mental health workforce, improve access to a natural and humanistic form of support, and lengthen and enhance the continuum of care with peer specialists and peer-led navigation services that bridge gaps in mental health care.
Congressional Bipartisan Fentanyl Prevention Caucus
Manifesto on the Hill!
Today, our Head of External Affairs, Patrick Flynn, presented to the Congressional Bipartisan Fentanyl Prevention Caucus alongside other experts and advocates, Dr. Donald Stader, Dr. Sally Satel, and Dr. Kevin Sabet.
Patrick spoke about the importance of expanding the behavioral health workforce, improving access to care, and enhancing the continuum of care with frontline peer support services that combat the devastation of the current opioid and fentanyl crises.
Learn more about the Fentanyl Prevention Caucus here.
New National Standards for Peer Support Workers
“States recognize the value that the peer workforce brings to behavioral healthcare and are exploring ways to support and advance these critical services” — SAMHSA spokesperson
SAMHSA recently released national model standards for certifying peer support workers. The primary goal of improving standards and certification processes for peer support specialists is accelerating the universal adoption, recognition, and integration of the peer mental health workforce across domains of the healthcare system. SAMHSA collaborated with federal, state, tribal, territorial, and local partners, including peer specialists, to develop national standards inclusive of substance use, mental health, and family peer certifications. These standards aim to mitigate the behavioral health workforce shortage by improving quality and access to a natural, humanistic, and effective form of care that is currently underutilized.
In March of 2022, President Biden announced his administration’s strategy to address our nation’s mental health crisis. This national mental health strategy seeks to strengthen system capacity, connect more Americans to care, and create a continuum of support — transforming our health and social services infrastructure to address mental health holistically and equitably. A major goal within this systemic strategy is facilitating the adoption and implementation of a broader and versatile peer support workforce across the spectrum of healthcare sectors.
Peer support services have gained recognition over the past several decades as a vital component of mental and behavioral health services. Peer support workers use their lived experience of recovery, combined with professional training and supervision, to assist people in initiating and maintaining recovery. Through shared understanding and mutual empowerment, peer support workers can fill the gaps in support that clinical care cannot reach. A robust body of empirical evidence support peer specialists’ effectiveness in a myriad of positive outcomes including increased treatment retention, improved access to social supports and other social determinants of health, as well as reduced misuse recurrence, criminal justice involvement, and recidivism to hospitalizations and residential treatment (see our prior post for references). These benefits would not only improve care and health outcomes but also significantly lower the overall cost of behavioral healthcare.
The need for standardized national standards arises from the growing demand for consistency, competence, and accountability in this evolving field. These standards act as a benchmark — ensuring that individuals seeking peer support receive the highest quality of care, regardless of their location. Additionally, issues including reimbursement and state license requirements have set up barriers that organizations face when attempting to employ the peer workforce. While the new standards do not substitute for any state certification, their goal is to hasten universal adoption, recognition, and integration of the peer mental health workforce across the country.
There are over 30,000 people who have overcome addiction and struggles with mental health that want to assist those who are currently struggling, Samir Malik, CEO of firsthand, told Behavioral Health Business. These national standards are a formative guide in the efforts to fulfill workforce gaps — and the growing need for peer support specialists to use their lived experience and versatile skillset to help individuals navigate their lives and stay on track with their self-directed goals and values. The model standards aim to standardize certification across the different forms of peer support — mental health, substance use, and family support — while recognizing the commonality and differences between them. SAMHSA outlines the education, hours of training, work experience, and examination requirements for peer support workers
The introduction of these new national standards on peer support certifications marks a significant milestone in the field of behavioral health services. These standards have the potential to elevate the quality, accessibility, reach, flexibility, and acceptability of peer support services — ensuring that individuals receive consistent, competent, and ethical care. As peer support continues to gain recognition and impact lives in its natural, humanistic form — the peer workforce will further solidify its position as an invaluable resource on the path to recovery and well-being.
Reach out to Manifesto directly at info@manifestohealth.com to learn more about how we can enhance your patients, members, or employees health and wellness for the long run.
Dr. Mullen's Dissertation Study: Mental Health Professionals’ Perception of Medications for Opioid Use Disorder
The DEA appears to have filed for a temporary extension of telehealth flexibilities for medications for opioid use disorder (MOUD) beyond the public health emergency.
Our Chief Clinical Officer & Cofounder, Dr. Patrick Mullen's study—recently published online in Philadelphia College of Osteopathic Medicine’s Digital Commons—may shed some light on why reinstating restrictions on MOUD is something we should reconsider:
- Medications for opioid use disorder work. The evidence is unequivocal: MOUD keep people alive and significantly improve treatment outcomes (with or without adjunctive therapy) *
- Currently, MOUD is markedly underutilized in opioid use disorder (OUD) treatment. Merely one-third of substance use disorder treatment centers offer any form of MOUD and only 30% of individuals with OUD (the small portion that are diagnosed and treated) receive any form of MOUD. *
- In this survey of OUD professionals (clinicians or researchers that work directly with individuals with OUD) aimed to examine characteristics of groups (clinicians vs. researchers, years of experience in the OUD field, and direct exposure to MOUD) in relation to their utility ratings of MOUD (how “helpful” they rated the use of MOUD in treating OUD)
- Statistically significant differences between groups were found. Researchers rated MOUD significantly more favorably than clinicians. Professionals with more than 10 years in the field rated MOUD more favorably than professionals with less than 10 years of experience.
- What do this study's results indicate? Researchers and longer-tenured professionals have more access, exposure, and contribution to the scientific literature as well as real-world experiences with the OUD population and are therefore more aware and supportive of the effectiveness of MOUD.
- The study’s results suggest that the perception of MOUD could be enhanced by an increase in training and education.
- Here are some suggestions: (a) Targeted training that emphasizes the efficacy of medications, portrays OUD as a treatable condition, and illuminates personal narratives of people who are effectively treated with MOUD; (b) Academic detailing that involves visits to health care providers by trained professionals who can provide tailored training and technical assistance specifically designed for MOUD education and; (c) Improvements in continued education requirements for SUD professionals and nonclinical support staff.
- While it is encouraging to see behavioral health startups (e.g., Workit Health, Eleanor Health, Quit Genius) aiming to improve access to MOUD, recent barriers demonstrate that the misguided stigma associated with OUD in general, and MOUD in particular, persist.
Find the full publication here: Dr. Mullen's Dissertation Transcript
Why Does Recovery Capital Matter Now More Than Ever?
Recovery Capital (RC) are the resources that people in recovery rely on to sustain and enhance their lives—internal resources such as coping skills, resiliency, and perseverance as well as external assets such as supportive relationships, peer support, and meaningful work/employment.
Although the term was coined over 20 years ago (Granfield & Cloud, 1999), RC’s utility is only recently getting the attention it deserves. RC can be categorized in the following domains: (a) personal capital (qualities such as resiliency); (b) social capital (networks and supports that the individual can draw from) and (c) community capital (resources from the individual’s local community such as affordable housing and training/employment opportunities; Best & Laudet, 2010).
Why does Recovery Capital matter now more than ever? RC transcends traditional health screening and offers a more comprehensive picture of how an individual is doing on their recovery journey—identifying both strengths and areas for growth. In other words, RC is a currency of recovery—a measure of how much recovery an individual possesses at a moment in time.
RC enables a more meaningful and comprehensive assessment of recovery—insights into indicators and predictors such as global health and wellness, nutrition, social connectivity, employment satisfaction, socioeconomic status, relationship health, educational interests, and skill-building.
For example, RC enables an individual in recovery and their care team (e.g., a Manifesto peer recovery coach) to gain well-rounded insights into their strengths and potential risk areas while tracking useful outcomes and informing targeted and timely interventions. At Manifesto Health, we use RC as our barometer for progress—enabling a higher level of personalization for our nonclinical support services (in stark contrast to the one-size-fits-all addiction treatment approach).
Moreover, RC provides other stakeholders in the measurement and outcomes of treatment (e.g., providers, payers) a valid, reliable and standardized tool. This holistic measure of recovery transcends the limited and reductive measures of old—such as only tracking substance use recurrence or treatment recidivism.
RC gets us closer to an empirically testable science of recovery—one that upends traditional addiction science that emphasizes pathology over strengths and capabilities. Capturing and measuring recovery pathways and trajectories is a work in progress in addiction research. RC offers an empirically-driven and culturally-appropriate method that can accelerate addiction science and identify the elusive indicators and predictors of recovery.
As the evolution of value-based care in behavioral health continues to emerge, measurement and outcome tracking will take on a new level of necessity—and for good reason! We cannot manage (i.e., change/improve/modify/test) what we don’t measure—and Recovery Capital measures what matters.
Behavioral Healthcare Industry Outlook Panel
Join us on May 19th for the first of our live webinar series, Behavioral Healthcare Industry Outlook, featuring leading voices in the behavioral health industry.
With an estimated one in four adults having a diagnosable mental health condition and over 60 million people using substances, the need for person-centered, culturally appropriate, high quality behavioral health treatment has become a top priority in the United States. These disturbing statistics have led to a nationwide push to enforce parity laws, prioritize health equity, and integrate physical and behavioral health. In addition to expanding access and proving the care being offered is effective, stakeholders in the behavioral health field are calling for a corresponding change to the reimbursement model, one where incentives are based on value instead of volume. The result has been an accelerated push towards Value-based Care (VBC) contracts.
Hear from the expert panelists:
Tony Rocchino, Former Health Insurance Executive
Serenna MacLachlan MS, MAC, CADC-III, QMHP, CEO, SLO Recovery Center
Stu Segal, Owner & Consultant, @Strategic Solutions in Health
Eric J. Gremminger, ICADC, SAP Gremminger, Co-Founder & CEO, ERPHealth
Mike Lifshotz, Chief Executive Officer, Hatch Compliance
Gregory Keilin, Co-Founder / Chief Strategy and Growth Officer, Prosperity Behavioral Health
Nick Jaworski, Chief Executive Officer, Circle Social Inc.
Ben Dittman, Senior Vice President, Partnerships - Kipu Health
Dan Hilferty Jr., Co-Founder & CEO, Manifesto Health
Moderated by Cori E. McMahon, Psy.D., NCCE, Chief Clinical Officer at ERPHealth
Sign up today: https://lnkd.in/g86_dCTi